
Ms Lucy Hicklin ENT, Mr Paul King chief executive Dystonia society UK, Dr Marie-Helene Marion neurologist and Carol Harris speech therapist. London living with dystonia event, on swallowing and speech problems on the 8th november 2014, London.
Every day we swallow solid food like a piece of bread, water and our own saliva. This vital function occurs most of the time without us being aware of it, as a reflex. But in fact swallowing is a very fine and precise mechanism, which can be disrupted in a number of neurological conditions, the most common and dramatic one occurring after a stroke, but also in dystonia.
A few definitions:
1- Doctors talks about swallowing difficulties as dysphagia, which is the difficulty moving food from mouth to stomach.
2- Swallowing difficulties can be severe leading to a misdirection of the food to the nose, or to the larynx (voice box) and the lungs, resulting in infection of the lungs called aspiration pneumonia (as the food has been sucked int the airways).
3- Swallowing difficulties are silent when there is no manifestation which will make the person aware of the swallowing problem, such as cough, choking, needed to drink to push down the food.
4- Swallowing difficulties are subclinical when the signs are so mild that they are overlooked such as cutting food into small pieces and taking a sip of fluid with each swallow.
What are the essentials for good swallowing?
1- Of course the machinery such as the tongue, the mouth, the throat (the pharynx) the voice box (the larynx), the oesophagus (gullet) have to be healthy. Issues apart from neurological problems, such as a tumour, could obstruct the swallowing process.
2- The nervous system has to be able to conduct in an orderly fashion the different sequences of the swallowing, like a conductor with his musicians; only one “ fausse note” can disturb the all process. It’s called neurogenic dysphagia.
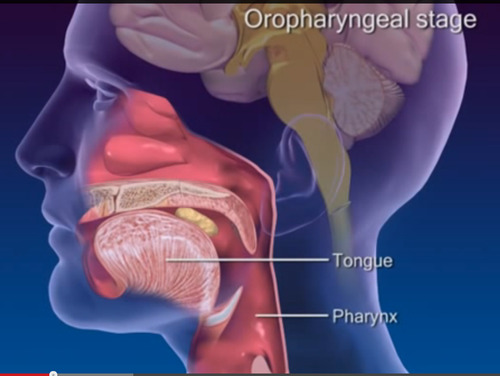
What are the sequences of the swallowing?
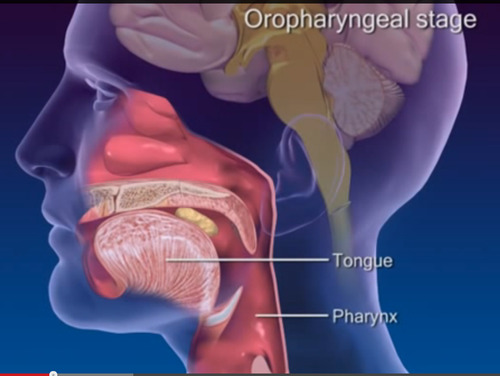
1- The oral phase: the food is collected in the mouth as a soft mass of chewed food, called a bolus.
2- The pharyngeal phase: the swallowing reflex is triggered by the bolus touching the back of the throat, which give a signal to the brain ( cortex and brainstem) to start the safe guard process: the airway needs to be protected by elevating and closing the larynx and by lifting the soft palate to close the back of the nose. The door to the oesophagus (the crico-pharyngeal sphincter) opens to let in the bolus which has been propelled downwards by the back of the tongue and the pharyngeal muscles.
3- The oesophageal phase. The bolus then passes though the gullet and into the stomach. This is under the control of the autonomic nervous system
How can swallowing difficulties be assessed?
1- -During a consultation, a speech therapist will examine the tongue strength, gag reflex, voluntary cough, and speech and perform a trial of swallowing (water, puree) and/or a 3 ounces (90 ml) water test.
2- FESS (fiberoptic endoscopic evaluation of swallowing).
A fine “spaghetti “( fibre-optic) tube, with a camera at the end, connected to a screen, is introduced by the nose and passed gently down to the throat. With the camera in place the patient is asked to swallow a food of different consistencies. The food is normally dyed blue or green to make it easy to see against the pink of the gullet. The speech therapist performing the test can see where it is going, particularly if it is getting stuck or going down into the airway (aspiration) .
3- Videofluoroscopy is video-radiography of the mouth, throat and oesophagus when the patient swallows a range of foods (biscuit, puree, yoghurt) and liquids that are coated in barium. The barium shows up on the x-rays (radio-opaque). On the video the radiographer can follow the trajectory of what has been swallowed.
4- Recording the swallowing process with electrodes in the muscles under the chin and movement sensors on the Adam’s apple can give a good indication of the timing of the different swallowing phases. It’s called an electrophysiological assessment.
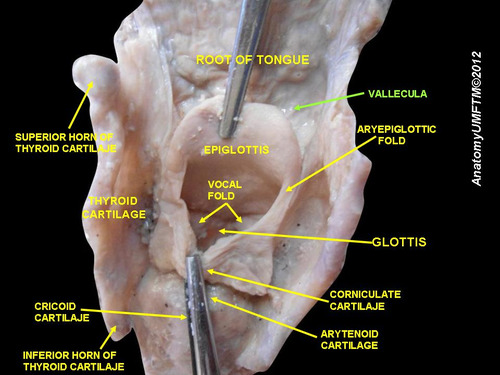
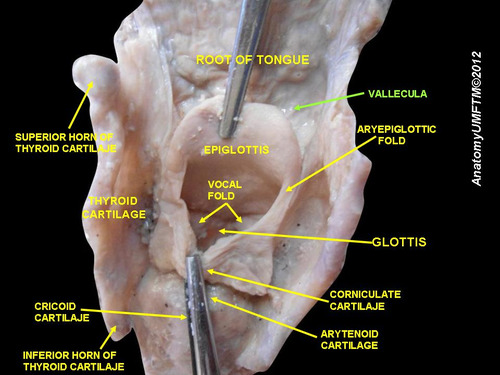
Posterior aspect of the base of tongue and larynx , after removing the pharynx http://commons.wikimedia.org/wiki/File:Slide10vvv.JPG#mediaviewer/File:Slide10vvv.JPG
What about swallowing difficulties in dystonia, in untreated patients?
Very few studies have addressed this topic. Most have concentrated on the swallowing difficulties in dystonic patients following treatement with Botulinum toxin injections.
I will present 5 studies of swallowing difficulties in patients with cervical and craniocervical dystonia, before treatment.
1-Riski et al (1990) studied 43 patients with cervical dystonia with videofluoroscopy and found that 51% of the patients had swallowing difficulties; in 16% the difficulties were subclinical (not known by the patient). The patients had mainly a delay in triggering the swallowing reflex and some residue in the vallecula (a groove, behind the base of tongue, usually cleared by the posterior movement of the base of tongue).
2–Comella et al (1992) studied 18 patients with cervical dystonia with videofluoroscopy before and after Botox injections; 11% patients had clinical symptoms of swallowing difficulties and 22% had radiologic signs of peristaltic abnormality.. after Botox (see below), the signs and symptoms of dysphagia in these patients did not change, but an additional 33% developed new dysphagic symptoms and 50% of the patients developed new peristaltic abnormalities by radiologic studies.
3- Munchau et al (2000) studied 12 patients with cervical dystonia undergoing selective peripheral denervation with videofluoroscopy. 90% patients had swallowing abnormalities with 58% subclinical. The patients presented as in the Riski’s study, with delayed initiation of the swallowing reflex and abnormal tongue base posterior movement, in particular in patients with saggital shift of the head.
The subclinical dysphagia was mainly cutting food into small pieces and taking a sip of fluid with each swallow.
4–Ertekin et al (2002) studied 25 patients with cranio-cervical dystonia with electrophysiological assessment. . 36% had clinical dysphagia and 72 % had abnormal swallowing on electrophysiological recording with again delayed swallowing reflex ; also the sphincter ( the crico-pharyngeal muscle) which opens the oesophagus was hyperactive, instead of being relaxed during swallowing to let the food going through.
Ertekin developed the concept of the dysphagia limit. In this simple test patients are asked to swallow volumes of water ranging from 1ml to 20mls. In patients with clinical swallowing problems only 1-10 mls can be swallowed in one go. In subclinical patients 10-15mls can be managed. All normal subjects could swallow 20mls in 1 gulp.
5-Cersosimo et al (2005) studied 20 pts with Meige syndrome with videofluoroscopy. 90% patients had abnormal swallowing compared to 40% in a healthy population of same age. They found also residue in the vallecula as in Riski’s study
What about swallowing difficulties in dystonia in Botox dystonic patients?
Botulinum toxin injections, by weakening adjacent muscles, have been responsible of transient dysphagia in dystonic patients.
The different types of dysphagia depending of the sites of the Botox injections have been detailed in a previous post.
Conclusion
Swallowing difficulties are often silent or subclinical in dystonic patients. Patients and doctors need to speak about them as these swallowing difficulties can be worsened by Botulinum toxin treatment administered for the treatment of the dystonia.
Maybe every injector needs to offer a drink to their dystonic patients before treating them! It may be well received…..

References:
Swallowing function in patients with spasmodic torticollis.; Riski JE1, Horner J, Nashold BS Jr; Neurology. 1990 Sep;40(9):1443-5
Dysphagia after botulinum toxin injections for spasmodic torticollis: clinical and radiologic findings.; Comella CL1, Tanner CM, DeFoor-Hill L, Smith C.; Neurology. 1992 Jul;42(7):1307-10
Prospective study of swallowing function in patients with cervical dystonia undergoing selective peripheral denervation; A Munchau, C Good, S McGowan, N Quinn, J Palmer, and K Bhatia; J Neurol Neurosurg Psychiatry. Jul 2001; 71(1): 67–72.
Oropharyngeal swallowing in craniocervical dystonia, C Ertekin*, I Aydogdu**, Y Seçil, N Kiylioglu, S Tarlaci, T Ozdemirkiran J Neurol Neurosurg Psychiatry 2002;73:406–411
Swallowing disorders in patients with blepharospasm.: Cersósimo MG1, Juri S, Suárez de Chandler S, Clerici R, Micheli FE. Medicina (B Aires). 2005;65(2):117-20
http://www.infodystonia.com/post/24333066534/swallowing-difficulties-after-botox-injections-what-to












You must be logged in to post a comment.